Health
July Kids’ Coverage Roundup
Updates on kids coverage in Utah: Kids are losing Medicaid/CHIP coverage, meanwhile Utah is still paying more to cover fewer people…and more!
Why are Utahns paying more to cover fewer people?
Under Utah’s current partial expansion plan (aka the “bridge plan”), Utah is paying 30% more to cover thousands of fewer kids and families on Medicaid. To date, around 34,000 new individuals have enrolled in Medicaid coverage, although at least 50,000 still remain in the gap, unable to afford coverage on their own and not offered it through their job. Utah has left at least $7 million in federal funds on the table so far-- funds that could be used to help more families get coverage and care. (New update: latest reports state the Trump administration will reject Utah's partial expansion. It's time to stop paying more to cover fewer people.)
Alarming Trend in Kids' Medicaid/CHIP Coverage
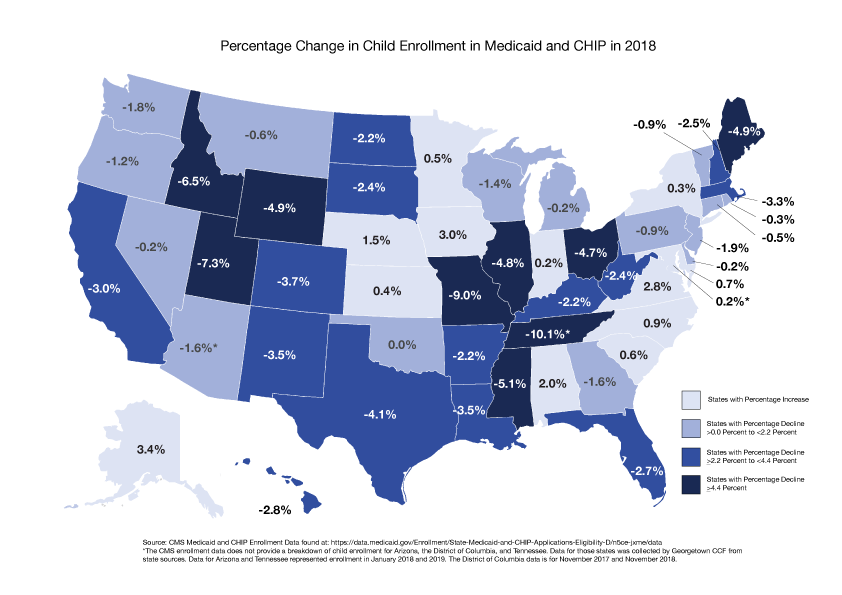
Utah kids are dis-enrolling from Medicaid/ CHIP at an alarming rate. At the July Utah Medicaid Advisory Committee meeting we learned that over 2,000 kids lost Medicaid/CHIP coverage last month. Such a steep drop cannot be explained by a strong economy alone. The number of Utah kids leaving CHIP/ Medicaid are among the highest in the nation. Both the Utah Department of Health and Department of Workforce Services have committed to doing additional investigation as to WHY kids are losing coverage. We greatly appreciate that they are taking this issue seriously and are working to find answers.
Utah Medicaid Advisory Committee Once Again Prioritizes 12-Month Continuous Eligibility- Let's Keep Kids Covered!
For the third straight year, the Utah Medicaid Advisory Committee prioritized 12-month continuous eligibility for children on Medicaid as one of their top funding requests to the Governor. 12-month continuous eligibility would allow more kids to get covered- and stay covered. Current Medicaid reporting requirements mean many kids unnecessarily lose coverage, with cascading negative impacts. This policy would protect kids and families. The Utah Medicaid Advisory Committee has continually prioritized this as a cost-effective, best practice to keep kids healthy, consistently voting in favor of the Utah Department of Health adopting this policy.

The Latest on Utah’s Medicaid Waiver
Utahns submitted a record 1,700 comments on Utah’s partial Medicaid expansion. Thanks to all who stood up for voter-approved full Medicaid expansion. Utahns voiced strong opposition to the proposed cuts, caps and barriers to Medicaid coverage which would leave many kids and parents without coverage or care. These comments send a message to state and federal officials and will provide the backbone for any future legal action.
Haven’t submitted a comment yet? There’s still time! Submit a comment here: www.utahchildren.org/comment

Breaking Down Data to Help All Families Thrive
Breaking Down Data to Help All Families Thrive
At Voices for Utah Children we start with the question, “Is it good for kids?” We advocate for data-driven policy and community solutions to improve the lives of all children. This data brief and case study examines why the collection, analysis and reporting of race and ethnicity data is critical to help drive policy solutions for Utah kids. If we only report on whole populations, we may overlook important racial or ethnic trends and disparities. By sharing outcome data for different racial and ethnic groups, we can help address systemic problems and ensure greater accountability in policymaking and public programs.
Case Example of Utah Native Hawaiian/ Pacific Islander Birth Outcomes
In Utah, there are nearly 38,00 Native Hawaiians/Pacific Islanders (NHPIs). The overall percentage of NHPIs living in Salt Lake City is greater than any other city in the continental U.S. The median age of Utah NHPIs is 20.2, making them one of the youngest populations in Utah.
In 2010, the Utah Department of Health Office of Health Disparities examined the infant mortality rate for the NHPI community for the first time. Previously, birth outcomes for the NHPI community had been reported together with birth outcomes for Utah Asian Americans. When grouped together, the infant mortality rate for the Asian American and Pacific Islander communities was lower than the state average at 4.6 deaths per 1,000 births, compared to the overall average of 5.2 deaths per 1,000 births.
However in 2010, when prenatal and birth outcomes for NHPIs were examined separately, the data told a very different story: Pacific Islander infants under one year had nearly twice the death rate (8.8 deaths/1,000 births) of infants statewide (4.5 deaths/1,000 births). While only 1.3% of all Utah infants were born to Pacific Islander mothers, their babies made up 2.5% of all infants who died. Other birth outcomes disparities among Pacific Islanders, including access to prenatal care, also surfaced.
These alarming findings underscored the importance of greater access to and breakdown of ethnic/racial data to understand population trends. In response, the Office of Health Disparities conducted additional research and investigation. OHD worked collaboratively with state and local partners to develop a community-based health promotion and education program to reach NHPI residents in Utah. The “It Takes a Village: Giving Our Babies the Best Chance” (ITAV) project raises awareness and addresses birth outcomes disparities in the context of Pacific Islander cultural beliefs and practices. The ITAV project has been designated a promising, innovative practice from national public health organizations. Results show that the ITAV project effectively raises awareness, improves knowledge, and increases self-efficacy among NHPI participants. In 2019, the University of Utah Department of Family and Preventive Medicine received funding to expand the ITAV project to St. George with the Southern Utah Pacific Islander Health Coalition, broadening the reach and impact of the project. In addition, the data disaggregation at the root of the ITAV project inspired other states, including California, to collect and report disaggregated health data for Native Hawaiians and Pacific Islander populations.
Moving Forward
All too often, public institutions and systems report data on whole populations or broad population categories. Yet this case study highlights how public institutions can also lead the way, rethinking current practice around data disaggregation, reporting and response.
Going forward, Voices for Utah Children is actively working to ensure that the data we share, such as the annual Kids Count Data book, can better disaggregate Utah demographics. We call upon more state and local public institutions and agencies to do the same. Our state agencies must continue to be leaders in data disaggregation to ensure families are getting the care they need. Disparities cannot be fully identified or addressed without adequate data and reporting.
It is equally important to ensure that disparities identified are met with culturally appropriate resources, investments and policy change. The ITAV project demonstrates how disaggregated data, coupled with community-based solutions, can help more families be empowered to change their health practices. While many factors influence health outcomes and trends, community-driven public health interventions, like the ITAV project, can play a significant role.
However, disparities in maternal and birth outcomes persist in Utah. NHPI mothers are still receiving less prenatal care than other populations in Utah. This points to the need to address more systemic inequities in access to care, insurance coverage and culturally-competent health care services. All mothers and infants in Utah deserve a healthy start, regardless of their culture or background. Policies that promote affordable, quality health care, including Medicaid coverage, access to prenatal services and mother-infant support programs can help improve the lives of all Utah moms, babies and communities.
To download a copy of the brief and references:
Why is Utah Cutting Back Care for Young Adults?
Young adults on Medicaid are being denied dental and vision care, mental health screenings and other benefits, just as they enter the work force and embark on the next chapter of their lives.
Baffled by this decision? So are we.
Utah is proposing several, unprecedented changes to its Medicaid program. These changes include limits on enrollment, work reporting requirements and per capita funding caps. But here’s one issue that has received less attention: Young adults on Medicaid are being denied their full benefits, including early detection and screening services, dental care, mental health and wellness care (known as the acronym, EPSDT). The Medicaid Act mandates that individuals enrolled in Medicaid have comprehensive EPSDT benefits up to age 21. The American Academy of Pediatric endorses it. But Utah has arbitrarily chosen to cut comprehensive benefits to 19 -20 year olds.
Advocates are told this is a cost-saving measure. But the evidence doesn't back this up. Early screening and detection services SAVE dollars. Why is Utah cutting the very benefits that help detect conditions before they escalate and cost the state more money?
-
Providing prevention, early detection, and treatment services for young adults insures that health problems are averted or diagnosed-- allowing young adults to focus on furthering their school, work and life.
-
Young adults’ brains continue to develop past their teenage years into their 20s. Access to things like vision, hearing and dental screenings, as well as mental health services, help young adults stay on track at a critical point in their development.
-
Cutting dental benefits for young adults makes it harder for them to find a job. Individuals living below the poverty level have reported that the appearance of their teeth and mouth had a negative effect on their ability to interview for a job.
-
We are in the middle of a youth suicide crisis. Now is not the time to cut back access to mental health screening and care for young adults. As 19-20 year olds prepare to make more adult decisions it becomes even more common for mental health issues to arise.
This state does not need to move forward with this harmful decision. It runs counter to Utah’s fiscal prudence, focus on cost-effective solutions, recent legislation protecting children’s health up to age 21, and the state’s own policies. The Utah Department of Health actually endorses the American Academy of Pediatrics Bright Futures guidelines, which recommend full comprehensive benefits for everyone up to age 21.
Many of the proposed changes to Utah’s Medicaid program are mandated by Senate Bill 96. But this isn’t one of them.
Utah has the opportunity to make a different choice, to support young adults as they become more self-sufficient, not turn our backs on them.
TAKE ACTION: Tell the Utah Department of Heatlh to protect comprehensive benefits for 19-20 year olds. Use this link to submit your comments by June 30th.
2019 Utah State of Children's Coverage Report, 100% Kids: Giving All Kids the Opportunity to Thrive
Report: 2019 UTAH STATE OF CHILDREN’S COVERAGE REPORT 100% Kids: Giving All Kids the Opportunity to Thrive
Executive Summary
Health insurance coverage provides children with the foundation they need to be healthy and thrive. When children have health insurance, they have better health outcomes, greater academic success and more economic opportunities later in life.
Utah lags behind the rest of the nation when it comes to covering kids. In Utah, 7% of all children are uninsured, compared to 5% nationally. While Utah has made significant strides over the years connecting more children to coverage, in the last year, Utah’s child uninsured rate has increased. In 2017, Utah was one of only nine states to see its child uninsured rate trend in the wrong direction.
Who are the uninsured children of Utah? They are overwhelmingly low-income. Typically, their parents are uninsured too. The majority are eligible for CHIP or Medicaid insurance, but not enrolled. Some are not eligible for insurance at all because of their citizenship or immigration status. They live across Utah, with a higher percentage of uninsured children living in rural areas. Some children may have never been insured; some may have had insurance and then lost it or had a parent dis-enroll them due to stigma or fear of enrolling in public health insurance programs. They come from all racial and ethnic backgrounds however, a disproportionate percentage of uninsured children in Utah are Latino, the highest in the nation. Some come from families experiencing intergenerational poverty, some are immigrants, refugees or asylum seekers, facing steep obstacles to their health and well-being.
But no matter who they are, they are all Utahns. When 7% of our child population lacks health insurance, we put Utah’s future at risk. Utah is at a unique moment to challenge the negative trends and demand that all children, no matter their background, zip code, citizenship or immigration status, can access affordable health coverage.
The 100% Kids Coverage Campaign is led by a diverse coalition of stakeholders. This multi-year campaign has a goal of ensuring all Utah children will have coverage. Guided by four over-arching policy recommendations, the Campaign proposes to change Utah’s health coverage landscape:
- Strengthen and protect Medicaid coverage for parents
- Keep kids covered all year round
- Support consistent outreach and enrollment support
- Cover all kids, regardless of background or immigration status
Through targeted policies, political and community engagement, we can ensure that all Utah kids have the health coverage they need to grow, thrive and succeed in life. We believe that it is possible for 100% of Utah children to have access to affordable, consistent health coverage. We invite you to join us and help us reach 100% together.
The full report can be downloaded below. For a free print copy please call Voices at 801-364-1182
100% Kids Coverage Campaign & Coalition Launch
100% Kids Coverage Campaign & Coalition Launch
Giving All Kids the Opportunity to Thrive
FOR IMMEDIATE RELEASE
Wednesday, May 22, 2019
CONTACT:
Ciriac Alvarez Valle
801-364-1182
Salt Lake City —A coalition of over 20 diverse stakeholder organizations will announce a campaign aimed at ensuring that all Utah children have health care coverage, regardless of background, geography, immigration status, or income this Friday, May 24that 10 am at the Voices for Utah Children office (details below).
Utah has one of the highest uninsured rates for children in the country. In the last year, Utah was one of only 9 states to see an increase in its child uninsured rate, up from 6% to 7%. Children of color and immigrant children are disproportionately affected, of the 71,000 children without health insurance, almost 43% are Latino children. The Campaign aims to reduce the disparities in coverage and ensure that every child has the ability to access affordable health coverage.
During the launch, Voices for Utah Children will share its new State of Children’s Coverage Report with detailed information regarding Utah coverage, disparities to care and barriers faced by immigrant families. The 100% Kids Coverage Campaign focuses on four main policy priorities: Protecting and fully expanding affordable coverage for parents and pregnant women; keeping kids covered all year round; helping families connect and stay covered; and covering all kids regardless of immigration status. More detailed information about the campaign can be found here: https://utahchildren.org/issues/100-kids-covered.
The report includes several stories and testimonies from immigrant families on the importance of health insurance. “If [our family] had medical insurance, I’d be a calmer woman, with less stress, and more happiness because I’d have my son in his therapies that he really needs,” said one Utah mother in the report.
“Our campaign is committed to ensuring that Utah is a place for all children to grow up healthy, regardless of immigration status,” said Ciriac Alvarez Valle, Health Policy and Community Engagement Fellow for Voices for Utah Children. “We are encouraged to have so many groups come together in support of getting Utah to 100% Kids Coverage.
The Campaign & Coalition Launch will be held on Friday the 24th at 10:00 AM at the Voices for Utah Children Office (747 E South Temple #100).
###
New report Finds Medicaid Expansion Leads to Healthier Mothers and Babies
A new report shows states that fully expanded Medicaid saw a sharp decline in the uninsured rate for women of childbearing age. Utah’s uninsured rate for women ages 18-44 was at 11.2 percent in 2017, according to a new report by the Georgetown University Center for Children and Families. In comparison, states that had implemented full Medicaid expansion had an average uninsured rate of only 9 percent. Utah recently received a waiver to begin partially expanding its Medicaid program. More Utah women will now be eligible for Medicaid coverage; however, following the decision of the Legislature and Governor to roll back the voter-approved expansion, thousands of residents will still remain without the health coverage they need, including prenatal care.
Medicaid expansion has played a key role in reducing rates of maternal death, decreasing infant mortality rates, and improving the potential for optimal birth outcomes that can increase the promise for a healthy childhood, according to the report. States that fully expanded Medicaid saw a 50 percent greater reduction in infant mortality, compared to non-expansion states.
“Health coverage before, during, and after pregnancy is essential to the health and well-being of both mother and child,” said Joan Alker, executive director of the Georgetown University Center for Children and Families. “Medicaid expansion is the single most effective way to help women of childbearing age get continuous health coverage during this critical stage of life.”
States that have expanded Medicaid have also decreased the likelihood that women’s eligibility for coverage fluctuates, resulting in losing and regaining coverage over a relatively short span of time. Breaks in health coverage, also known as “churn,” can disrupt care and cause existing health conditions to become more serious and more difficult and expensive to treat, according to the report.
“The message of this study is clear: Medicaid expansion can protect the lives and health of women and their babies, especially women of color who are at higher risk for a range of poor outcomes,” said Dr. Rahul Gupta, Senior Vice President, and Chief Medical and Health Officer at March of Dimes. “If mom isn’t healthy, then her baby is at higher risk for a whole host of health consequences. If she’s healthy, however, that baby has a much higher likelihood of getting the best possible start in life.”
The American College of Obstetricians and Gynecologists recommends that women have access to continuous coverage prior to becoming pregnant and 12 months postpartum to reduce preventable adverse health outcomes.
“OB-GYNs have long recognized that continuous, quality and affordable medical care is vital to the health and wellbeing of our patients,” said Barbara Levy, M.D., Vice President of Health Policy at ACOG. “This important research demonstrates that Medicaid expansion plays a critical role in reversing the steadily rising rates of maternal mortality in the United States by ensuring women have access to the care they need before, during and after childbirth. As many as 60 percent of maternal deaths are preventable. Therefore, ACOG encourages both expansion and non-expansion states to continue working toward Medicaid policies that fill the gaps in coverage to improve health outcomes for women and babies.”
Research shows that health coverage prior to pregnancy helps address risk factors such as obesity, diabetes and heart disease and improves access to timely prenatal care. In Utah, new mothers typically lose Medicaid coverage 60 days postpartum. When mothers abruptly lose health coverage so soon after giving birth, it can force women to abandon medication or other ongoing treatment they may need, including support for postpartum depression, which can affect up to one in seven Utah women.
“As Utah begins implementing its partial Medicaid expansion, we know that there is more we can and need to do to make affordable health insurance available to all Utah residents.” said Jessie Mandle, Senior Health Policy Analyst with Voices for Utah Children. “When women are shut out of affordable coverage because they do not qualify for Utah’s partial expansion, or because they experience disrupted care, this impacts the whole family. This report makes clear that full Medicaid expansion, without caps, barriers or disruptions, is critical for the health and well-being of Utah moms and kids.”
See the full report: https://bit.ly/2JPfa9N
Healthy kids do better in school. Research shows that school-based care plays a critical role ensuring kids can stay healthy and learn. Thanks to collaboration and vision from our state leaders, Utah is making strides to help more children connect with care at school.
- During the 2019 Legislative Session, schools received new funding to increase school-based mental health services, including school nurses. School nurses can help identify a mental health condition before it escalates and connect kids with appropriate care.
- Utah is one of a handful of states currently exploring innovative ways to leverage Medicaid funding in schools. By leveraging Medicaid, schools could access additional funding to offer preventive health services such as dental care or mental health services.
- Schools help enroll kids in affordable health insurance. School-based Medicaid/ CHIP outreach and enrollment support is one of the most important ways kids can connect with coverage. Learn more about getting enrollment support at your school!
- School-based clinics, or school-based health programs, are critical ways to help kids access care. For example, school-based oral health programs help ensure kids get preventive dental care. Oral health pain is one of the top reasons kids miss school. New policies, such as teledentistry reimbursement, can ensure the long-term sustainability of school-based health care programs.
Learn more about...
- How newly eligible people can enroll in Medicaid and how you can help connect families with coverage.
- What’s happening with Utah’s waiver requests to add additional reporting requirements, caps on enrollment, funding limits and other harmful changes to Utah Medicaid that undermine the expansion we voted for.
- How you can help STOP these harmful changes to Medicaid, and how your input during the forthcoming public comment period makes a difference.
Check out this recent slide show presentation on Utah’s Partial Expansion to learn more ! ![]() Utah's Partial Medicaid Expansion presentation
Utah's Partial Medicaid Expansion presentation
All Utahns deserve access to affordable coverage without barriers, cuts or caps.
Voices for Utah Children’s Response to CMS Approval of Utah’s Partial Medicaid Expansion
Voices for Utah Children’s Response to CMS Approval of Utah’s Partial Medicaid Expansion
Voices for Utah Children is dismayed by the Centers for Medicare & Medicaid (CMS)’s decision today. While we are encouraged that some Utahns will be able to access needed care, too many Utahns will still be left without health coverage.
In November of last year, Utah voters passed a plan to close the coverage gap and fully expand Medicaid up to 138% of the federal poverty level, bringing federal tax dollars home to Utah. However, during the 2019 Legislative Session, the Utah Legislature rejected the will of voters and rolled back that plan, including the federal funds that came with it, despite outcries from the public, providers, patients, community leaders and many of its own legislators.
Today CMS chose to approve the Legislature’s more expensive partial Medicaid expansion plan -- a plan that will cost Utah taxpayers more, cover fewer people, impose harmful barriers to care and caps on enrollment for low-income Utahns. This plan creates a dangerous precedent for our Medicaid program and gambles with Utah taxpayers’ hard-earned dollars.
Of particular concern in this waiver:
- It doesn’t add up. The waiver forces Utah to spend more of its own money to provide health coverage to fewer people. Utah will only receive $2.30 in federal funds for every state dollar spent on Medicaid instead of $9.30 in federal funds for every state dollar spent under full Medicaid expansion.
- It’s dangerous. Medicaid is designed to help in times of crisis, allowing states to respond to public health emergencies, natural disasters, and to provide support during economic downturns. Limiting the number of people who can enroll in the Medicaid program could leave many vulnerable Utahns shut out from health coverage when they need it most.
- It doesn’t work. Research shows that work reporting requirements do nothing to help people find work, but instead create unnecessary red-tape and program complexities that result in hard-working, qualified Utahns losing their health coverage.
CMS’ approval of this partial expansion waiver will leave many unable to access affordable coverage and creates more health care obstacles for both parents and children. When parents’ coverage is in jeopardy, kids’ coverage is also at risk. While Voices for Utah Children is encouraged that some Utahns will get coverage starting on April 1, this plan undermines voter-approved full Medicaid expansion. Utahns deserve better; all Utahns deserve access to affordable health coverage without caps, unnecessary red-tape, and stumbling blocks.
For more information please reach out to Jessie Mandle, the Senior Health Policy Analyst at .
####
Helping Utah Kids Thrive in Every Zip Code: How the 2019 Session Addressed the Social Determinants of Health
This past Legislative Session, we saw many exciting bills aimed at helping kids grow up in safer and healthier environments. Not all of these bills passed, but they helped bring attention to important social determinants affecting kids’ health outcomes. No matter where a child lives, ALL Utah kids should have the chance to be healthy and succeed.
Getting Kids Outside
Several bills promoted kids’ access to Utah’s parks and outdoors, especially low-income kids and kids of color who traditionally have not had the same access to outdoors recreation. HCR 4 was a bipartisan resolution declaring Utah's Every Kid Outdoors Initiative. It declared that “it is critical for the well-being and development of Utah's children that we promote a healthy, active childhood filled with outdoor experiences for Utah's children.”
SB 222 created the Utah Children's Outdoor Recreation and Education Grant Program, which helps underprivileged or underserved kids have access to outdoor recreational opportunities and education, and encourages kids to engage in hand-on and nature-based learning and play.
Access to Safe Drinking Water for All Kids
Making sure kids have safe drinking water at school is critical to kids’ health. Staying hydrated should not make our kids sick- or impede their development. HB 360 would have made sure schools and childcare regularly tested their water for safe lead levels, while also providing mitigation funds. As Dr. Claudia Fruin said ‘"Utah has been extremely behind the times in lead awareness and testing initiatives." HB did not pass, but we will continue to elevate this important issue.
Helping more kids walk, bike or roll to school safely is important for kids’ physical, mental and emotional well-being. It keeps our kids active and decreases traffic around schools too. HB 208 helped to ensure the sustainability of Utah’s Safe Routes to Schools Program.

Addressing the Social Determinants of Health in Early Childhood
What if efforts to help our youngest children included connecting more kids with heathy foods, safe and affordable housing, and accessible transportation? SB 83 would have done just that, drawing on existing community strengths to help improve health outcomes for our youngest Utahns. Unfortunately, this bill did not pass, but it sparked important conversations about innovative and collaborative ways to help Utah families.
This is only a handful of the bills that addressed the social determinants during the 2019 Legislative Session. We also saw some important steps for families’ access to healthy food. Meanwhile, clean air and affordable housing were also hot topics during the Session with significant impacts for children’s health and well-being.
Even though the 2019 Session is over, we will keep working on these issues all year long and look forward to joining with our partners around the state. Utah kids in every zip code need to be able to grow, learn and play in heathy communities.