Health
Utah Parents and Families Would Benefit from Medicaid Expansion
 A joint report by the Georgetown Center for Children and Families and Voices for Utah Children finds that:
A joint report by the Georgetown Center for Children and Families and Voices for Utah Children finds that:- In Utah, uninsured parents account for over one third of the population potentially eligible for health coverage if the state expands Medicaid. If Utah does not move forward with Medicaid expansion, or an alternative proposal like Governor Gary Herbert’s Healthy Utah Plan, a significant coverage gap for parents living with dependent children will remain uninsured
- Of low-income, uninsured parents, working parents who are 26 to 49 years old and have school-aged children (6 to17 years old) are most likely to be helped by Medicaid expansion in Utah. Of those parents that could benefit from extended Medicaid eligibility, more than two-thirds (68 percent) are employed.
- Covering parents in Utah offers the state an opportunity to help its children by reducing their uninsured rate, enhancing a family’s financial security, and improving the health of parents. Utah ranks 43rd in the U.S. for percent of uninsured children; consequently there is significant room for improvement.
The complete repert is available here:
Utah Parents and Families Would Benefit from Medicaid Expansion
Learn More and Contact Lawmakers: http://bit.ly/HealthyUtah
Uninsured Rates High for Hispanic Children
Utah has Highest Uninsured Rate for Hispanic Children in the Nation
Every child in Utah should have a chance to succeed. When it comes to setting up a child for success, few things matter more than good health. It starts when their mothers get prenatal care. It continues with regular checkups after they are born to treat and, more importantly, prevent illness. Good health care helps children reach important developmental milestones and enter school ready to learn. Coverage is essential to children reaching their full potential. Unfortunately, too many Utah children are uninsured. This is particularly true for Hispanic children in our state.
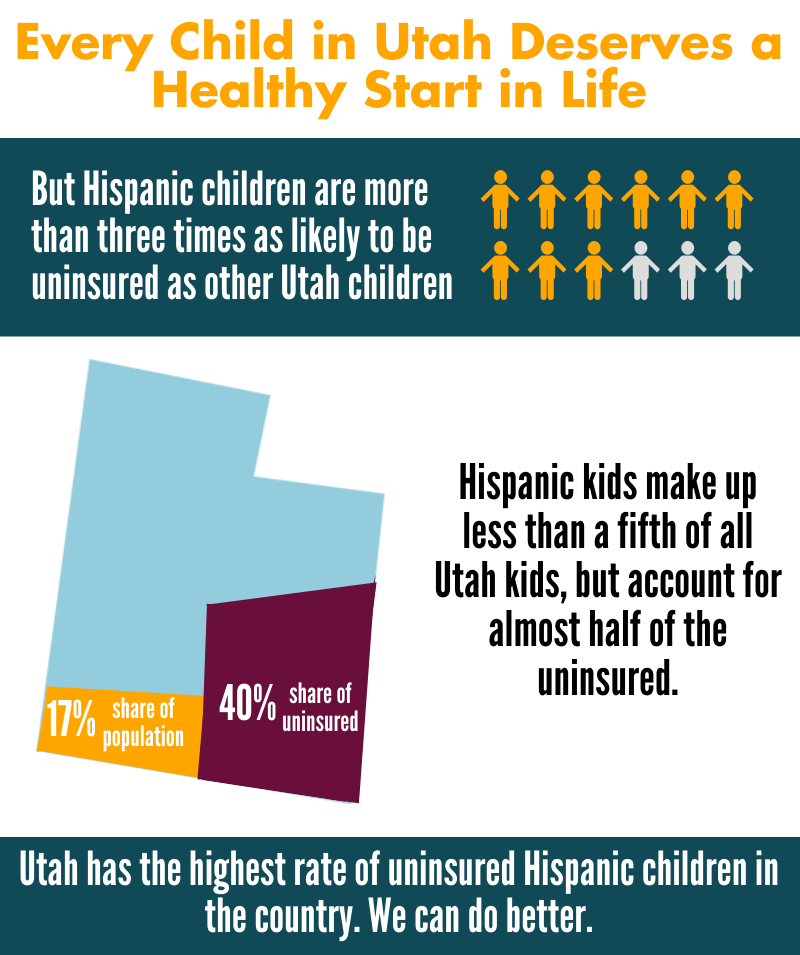 • 22.2% of Hispanic children are uninsured in Utah. This is the highest rate in the nation by far and is twice as high as the national average for Hispanic kids of 11.5%.
• 22.2% of Hispanic children are uninsured in Utah. This is the highest rate in the nation by far and is twice as high as the national average for Hispanic kids of 11.5%.
• 22.2% of Hispanic kids are uninsured compared to only 7% of non-Hispanic children. This 11 percentage point disparity is the largest disparity in the country. Nationally, the average disparity is only 5 percentage points.
• Hispanic children make up 16.9% of Utah’s total child population but account for 39% of the uninsured children in the state. Of the 84,891 uninsured kids in Utah, 33,531 of them are Hispanic.
• Utah’s overall uninsured rate for kids is 9.5%, ranking us 41st (highest being worst) in the country. The national average is 7.1%. If we reduced our Hispanic uninsured rate to the national average of 11.5%, Utah’s overall uninsured rate for kids would drop to 7.5% and Utah would have the 19th best uninsured rate in the country for kids.
If we want more children to succeed in life, we must secure coverage for more of our children, regardless of ethnicity or race. We can begin to remove hurdles facing uninsured Hispanic children and set all of Utah’s children on a path to success by implementing a few first steps:
• Restore outreach funding for Medicaid and CHIP;
• Make it easier for children to keep their health coverage by implementing 12 month continuous eligibility;
• Remove the Medicaid and CHIP five year waiting period that legal immigrant kids must endure before enrolling in these programs.
Printer-friendly version of this factsheet:
Using Pay for Success to Finance Nurse Home Visiting
 Pre-term and low birthweight infants face significant risks for medical and developmental disabilities which are expensive to government and private entities throughout a child’s life. Nurse home visiting, in which nurses and peer counselors provide support and education to high-risk pregnant women in their homes, have had excellent results over the past 30 years in preventing poor birth and long-term outcomes. Such programs that could significantly reduce state expenditures.
Pre-term and low birthweight infants face significant risks for medical and developmental disabilities which are expensive to government and private entities throughout a child’s life. Nurse home visiting, in which nurses and peer counselors provide support and education to high-risk pregnant women in their homes, have had excellent results over the past 30 years in preventing poor birth and long-term outcomes. Such programs that could significantly reduce state expenditures.
This paper, co-authored by Voices for Utah Children Early Childhood and Education Senior Policy Analyst Janis Dubno, explains how Pay for Success (PFS) finance could be used to pay for expanding nurse visiting programs. PFS finance involves a partnership between philanthropic and business entities (organizers and investors) and governments to provide performance-based investments in social programs, with payments made to the investors from cost avoidance savings that governments enjoy as a result of the program, or because the program meets certain prespecified outcome improvements. The key idea in a PFS project is that private investors (the managed care organization and/or senior and subordinated lenders) are repaid only from success payments, amounting usually to 80% to 90% of total cost avoidance savings.
This is the latest in a series of ReadyNation papers on using Pay for Success (PFS) social impact finance to improve early child health and education outcomes. This paper focuses on using PFS finance to scale-up effective early health interventions. PFS is a new financial and contracting arrangement that increases investment in evidence-based programs resulting in measurable social outcomes. Savings from these outcomes can repay investors and fund continued services. ReadyNation is leading a project to provide technical assistance to state and city teams developing PFS contracts. See www.ReadyNation.org/PFS.
For more information, read the complete paper:
Early Health “Pay for Success” Social Impact Finance: Scaling Up Prenatal Health Care in Virginia
Janis A. Dubno MBA, Robert H. Dugger PhD, Debra L. Gordon MS, David Levin MD, and Philip A. Peterson FSA
Nurse Family Partnership
Nurse Family Partnership (NFP) is a voluntary evidenced-based community health program that provides ongoing home visits (from pregnancy through age 2 of the child) from a registered nurse to low-income, first time mothers to provide the care and support they need to have a healthy pregnancy, be a responsible and caring parent, and to become more economically self-sufficient. A nurse visits the women approximately weekly and bi-monthly during their pregnancy and after birth, and then monthly visits during the first two years of their children’s lives. The program is a two-generation intervention and improves outcomes for both the mother and the child. NFP produces very strong outcomes for very high risk, low-income populations.
Economic analyses performed by the Washington State Institute for Public Policy, the Brookings Institute and the Rand Corporation determined that NFP provides a return on investment for taxpayers of $2.37 to $5.70 (high-risk population) per $1 invested in the program.
Download the printer-friendly report:
Nurse Family Partnership
Proven Outcomes
National outcomes associated with NFP, verified through independently evaluated randomized controlled trials, include long term family improvements in health, child welfare, education and self-sufficiency. When brought to scale, NFP can achieve:
• 23% reduction in smoking during pregnancy
• 26% reduction in pregnancy-induced hypertension
• 18% reduction in first pre-term births
• 58% reduction in infant deaths
• 30% reduction in second teen births
• 37% reduction in childhood injuries treated in emergency departments up to age 2
• 30% reduction in child maltreatment
• 38% reduction in language delay of the child by age 2
• 45% reduction in crimes and arrests, ages 11-17
• 51% reduction in alcohol, tobacco and marijuana use, ages 12-15
• 15% reduction in TANF and Food Stamp payments
• 9% reduction in Medicaid costs through age 1
Locally, Salt Lake County has a small NFP program. In 2012, 10.68% of the comparable Medicaid clients had a preterm delivery, compared to 7.5% of NFP clients, a reduction in incidence of 30%. Preterm babies require expensive medical services and a 30% reduction in incidence results in significant cost savings to Medicaid. In addition, the following outcomes for the mother have been documented in Salt Lake County:
• 52.5% increase in employment of clients younger than 18 after starting the program
• 18.9% increase in employment of clients 18 and older after starting the program
• 40% decrease in maternal smoking
• 50% reduction in reported incidence of domestic violence during pregnancy
Government Cost Savings and Avoidance
The outcomes listed above produce significant cost savings in Medicaid, Criminal Justice, Child Welfare, Food Stamps and TANF. Based on national data, Medicaid is the largest recipient of cost savings per family served (55% of cost savings accrue to Medicaid).
Nurse Family Partnership in Utah
The Office of Home Visiting in the Utah Department of Health received $1,097,713 in federal funding through the Maternal, Infant and Early Childhood Home Visiting (MIECHV) Program for Fiscal Year 2013. Of that, $300,000 was allocated to Nurse Family Partnership to serve 75 families in Salt Lake County (the remaining $700,000 was allocated to Parents as Teachers (PAT) - a home-visiting school readiness program). The average cost per family per year for NFP is $4,000. In 2012 (the most recent data available), 4,867 mothers were eligible for NFP statewide. Based on this, an investment of $19,468,000 would be necessary to serve all eligible families.
Recommendation
Voices for Utah Children recommends an ongoing state appropriation of $2,000,000 per year for Nurse Family Partnership, to serve 500 high risk, low-income first time mother statewide. To date, 21 states have appropriated state funds for NFP and/or home visitation.
More Information
New Report on States’ Oversight of Health Plan Network Adequacy
The bottom line? State regulation of network adequacy has a long way to go to protect consumers and ensure they have appropriate access to care. Below are highlights from the survey responses:
- Most states have not adopted the NAIC’s Managed Care Plan Network Adequacy Model Act.
- Most states monitor network adequacy primarily or only through consumer complaints. Unfortunately, this is an inadequate source of data because many consumers do not know they should communicate complaints to their state DOI (and most probably don’t know they have a DOI).
- While most states agree consumers need better information about plan networks and the risks and costs associated with out-of-network care, they report struggling to provide consumer-friendly resources on network issues.
- Just over one-third of states have requirements that PPOs update their provider directories on a regular basis.
- Overall, states have more regulatory authority over HMOs than they do over PPOs. They have even less authority over newer managed care products, such as “Exclusive Provider Organizations” or EPOs.
- Less than one-half of states have limits on balance billing.
- States rarely take enforcement actions against plans for problems related to network adequacy.
In light of these survey results, and the NAIC’s ongoing effort to revise its model act on network adequacy, the consumer representatives include in the report a set of recommendations for improved oversight, such as:
- Expand the scope of network adequacy regulations to encompass all types of network plans, including HMOs, PPOs, EPOs, Point of Service (POS) plans, and those using multi-tiered provider networks. Network adequacy regulations should also be flexible enough to accommodate new and emerging types of network formulations, such as Accountable Care Organizations (ACOs).
- Establish quantitative, state-developed standards for meaningful, reasonable access to care.
- Require insurers to submit access plans to DOIs for approval, to ensure that consumers are protected from network deficiencies.
- Ensure consumers have sufficient information to identify and select among broad, narrow, or ultra-narrow networks.
- Require all plans, not just Qualified Health Plans (QHPs) to include access to Essential Community Providers.
- Require that consumers be protected from balance billing in emergency situations and when receiving services from non-network facility-based providers in an in-network facility.
- Require health plan directories to be updated regularly and publicly available.
- Create special enrollment opportunities for consumers to move to a new plan if they rely on incorrect information published in the plan’s provider directory, their primary care provider becomes a non-participating provider, or a covered person in the midst of a course of treatment loses access to their specialty care provider or facility.
- Adopt standardized reporting requirements to monitor the frequency of use of out-of-network services.
A Two-Generation Strategy: Healthy Parents and Healthy Kids
While the vast majority of low-income families with children have at least one full-time worker, most do not qualify, or cannot afford, employer or individual market health insurance plans. Public health coverage programs can equally be out of reach. In most states, Medicaid and CHIP provide coverage to children and pregnant women, but largely exclude parents. However, an extensive body of research shows that when these programs provide coverage to both children and their parents, the entire family benefits.
Download the printer-friendly version of the report here:
A Two-Generation Strategy: Healthy Parents and Healthy Kids
Obviously, covering low-income parents increases their own insurance coverage and access to care. But the benefits do not stop at mom and dad. When parents have access to Medicaid, their Medicaid and CHIP eligible children are much more likely to get enrolled in coverage. Further, parental Medicaid coverage leads to improved use of health care for children, such as preventive care.
Parents living in states that have expanded Medicaid have seen nearly a 33% drop in the rate of parents living without health insurance. States that have not expanded Medicaid have seen no significant change in the rate of uninsured parents.
Medicaid Expansion: Parents and Children Benefit
Partly in reaction to this research, the Affordable Care Act (ACA) required states to move from Medicaid’s old categorical and individual centric approach to a more family centric program that would provide coverage to low-income children and parents alike. The 2012 United States Supreme Court decision that upheld the overall constitutionality of ACA, changed this section of law. Instead of mandating that states provide adults Medicaid coverage, the Court gave states the option to provide Medicaid coverage.
Over half of the states, including the District of Columbia, have expanded Medicaid for parents and other low-income adults. Unfortunately many states, including Utah, have not yet decided to expand Medicaid coverage to adults—and as a result, retained their individual centric Medicaid programs and higher rates of uninsured adults.
How Expansion Would Help Utah Families
Studies have repeatedly shown that health care coverage has a myriad of positive effects for families. Whether that coverage be private employer plans or a public Medicaid program, families’ financial security, ability to work, and the health of parents and children improve when adults have health insurance.
People with Medicaid coverage fare much better than uninsured on measures of access to care, utilization, and unmet health needs. Children enrolled in Medicaid, for example, are more likely to receive well-child care and are significantly less likely to have unmet or delayed needs for medical care, dental care, and prescription drugs due to cost.
Research suggests that Medicaid coverage has similar benefits for adults. Mothers covered by Medicaid are much more likely than low-income uninsured mothers to have a usual source of care, a doctor visit, a dental visit, and to receive cancer screening services. Adults covered by Medicaid are more likely than uninsured adults to report health care visits overall and visits for specific types of services. They are also more likely to report timely care and less likely to delay, or go without, needed medical care because of cost.
Further, out-of-pocket spending would decrease dramatically for low-income uninsured adults—almost four-fold on average, if they had access to Medicaid.
Recently, the Oregon Health Insurance Experiment has provided real life evidence about the positive impact of Medicaid coverage for low-income uninsured adults. Oregon had a lottery for a limited number of a slots in their Medicaid program for adults. This provided researchers the opportunity to look at the differences between adults who received Medicaid coverage and those who remained uninsured. Results from the Oregon experiment found that:
• 70% of enrollees were more likely to have a regular place of care
• 55% of enrollees were more likely to have a regular doctor
• Catastrophic out-of-pocket spending (health costs that exceed 30% of income) was nearly eliminated
• Any type of medical debt was reduced by more than 20%
Expanding coverage could have a direct impact on the health of children as well. Low-income adults are generally sicker than higher income adults. They suffer from increased likelihood of depression and other health issues that can lead to greater risk of their kids experiencing toxic stress. Medicaid expansion may help reduce this risk.
Unfortunately, low income adults in Utah are not experiencing these benefits of health coverage because the state has not yet chosen to expand Medicaid.
The data shows this is a significant problem in Utah where the story of uninsured adults is starkly different than the story of uninsured kids. Thirty-nine percent of adults below 138% of poverty and 43% of adults below poverty are uninsured in Utah. This compares to an uninsured rate of only 19% for adults with incomes above 138% of poverty.
The experience that states have had with children shows that providing access to Medicaid can dramatically reduce uninsured rates. The uninsured rate for children in Utah in households with incomes below 138% is only 18%.
The impact of Medicaid expansion does not stop with the adults who would gain coverage. Although much of the advocacy efforts surrounding Medicaid Expansion have focused only on the individual adults who would gain coverage, the reality is that over half of the expansion population is in a family (two or more related individuals), and nearly 40% are parents of children under the age 18. Providing health coverage to these adults in families will have a positive impact on everyone in that family.
Another misconception about the expansion population is their employment status. The fact is that 87% of families who would benefit from expansion include at least one working parent and 61.5% have at least one parent working full-time.
Unfortunately these families either do not have an offer of employer sponsored coverage, or cannot afford the employer sponsored insurance that is available. Only 29% of adults below 138% of poverty are enrolled in an employer sponsored health insurance plan.
Conclusion
Expanding Medicaid in Utah will strengthen Utah families. The improved health and financial security from providing health coverage to parents will greatly improve the opportunity to stop the cycle of intergenerational poverty.
Voices for Utah Children is proud to be a part of the Aspen Institute Ascend Network. The goal of the Aspen Institute Ascend Network is to mobilize empowered two-generation organizations and leaders to influence policy and practice changes that increase economic security, educational success, social capital, and health and well-being for children, parents, and their families. Learn more at http:/ /ascend.aspeninstitute.org/network
Healthy Utah Poll Results
 The Healthy Utah Poll was commissioned by a group of Utah civic groups interested in gauging support for Governor Herbert’s Healthy Utah plan. The poll was conducted by Dan Jones & Associates on a sample of 623 Utah voters during May and June, 2014. The full data and methods were then shared with Notalys for independent analysis. Notalys also consulted with the Dan Jones project leader on the development of the survey instrument. This report is the first set of research findings based on the poll. Complete poll results are found in this report along with a description of methods and an analysis of the results. The poll gives a clear and compelling summary of how Utah voters see the Healthy Utah plan, particularly in comparison to other options, such as a full Medicaid Expansion.
The Healthy Utah Poll was commissioned by a group of Utah civic groups interested in gauging support for Governor Herbert’s Healthy Utah plan. The poll was conducted by Dan Jones & Associates on a sample of 623 Utah voters during May and June, 2014. The full data and methods were then shared with Notalys for independent analysis. Notalys also consulted with the Dan Jones project leader on the development of the survey instrument. This report is the first set of research findings based on the poll. Complete poll results are found in this report along with a description of methods and an analysis of the results. The poll gives a clear and compelling summary of how Utah voters see the Healthy Utah plan, particularly in comparison to other options, such as a full Medicaid Expansion.
Download the complete report:
Key findings from the poll analysis
Widespread Support
- When compared with the option of doing nothing, 88% of Utah voters prefer the Healthy Utah plan, and 70% prefer Healthy Utah compared to a full Medicaid expansion.
- Healthy Utah has strong support across the state and among all demographic groups. Support is high for all age, education, race, gender, education and income categories.
No Partisan Divide
- Conservative Republicans support Healthy Utah. Among voters who identify as Republicans, 64% of those who are “very conservative” support the Governor’s plan, while just 13% oppose the plan.
- In general, support among Republicans is higher for Healthy Utah than it is among Democrats, since more Democrats favor Medicaid expansion.
Support for Affordable Health Care
- About 9% of likely voters are currently uninsured, even after healthcare.gov went into effect. A majority (54%) of voters know someone who is uninsured.
- Utahns think health insurance is very important, and, more surprisingly, 83% believe “all legal Utah residents should have access to affordable health insurance.”
- Utah voters believe that individual responsibility is important when it comes to insurance, but they are also supportive of government assistance for those who cannot afford coverage. Of the
- 65% of voters who agree that “individuals and families should generally be responsible for meeting their own healthcare needs,” 80% also agree with the statement that “individuals who are unable to afford health insurance should receive help from government sources.”
- Utahns are not opposed to a federal role in health care. 71% believe it is appropriate for the state to accept federal assistance in health care.
Support for Healthy Utah Plan Features
- A significant majority of voters are interested in the issue of health care, but only about 40% have heard of the new Healthy Utah plan thus far. When the details of the plan are provided, voters are in strong support.
- Utah voters strongly support the individual features of the Healthy Utah plan. Respondents say that the following features of the plan make them more likely to support it than they would otherwise:
- 59% are more likely to support the plan because it requires individuals to pay premiums and co‐pays (10% are less likely).
- 59% are more likely to support the plan because it provides private health insurance for people with low incomes rather than enrolling them in traditional Medicaid (14% are less likely).
- 68% are more likely to support the plan because it allows greater flexibility for how Utah spends federal dollars than allowed under traditional Medicaid (10% are less likely).
Opposed to Inaction
- The strongest consistency in the poll is that voters are very opposed to the status quo of doing nothing. Democrats are more inclined to do a Medicaid expansion, while Republicans support Governor Herbert’s plan. But both groups oppose the status quo. In a three‐way comparison, only 6% of the state voters prefer doing nothing.
- If Healthy Utah is rejected by federal officials, 65% would support a new Utah‐specific solution, and 28% support a Medicaid expansion. Only 7% would favor doing nothing.
- And, 54% of voters indicate they would be more likely to vote for legislators who support Healthy Utah. Only 14% indicate they would be less likely to vote for a legislator who supported the plan.
Poll Take‐Aways
- Utahns are overwhelmingly supportive of the features of Governor Herbert’s Healthy Utah plan.
- Utahns value individual responsibility, but both Republicans and Democrats are strongly supportive of a government role in assisting low‐income individuals to obtain health insurance.
- What Utahns are against, more than anything, is doing nothing.
The Economics of the Healthy Utah Plan: A Preliminary Analysis
This economic analysis of the Healthy Utah Plan was funded by Voices for Utah Children and completed by Sven E. Wilson, PhD. The Healthy Utah plan is the governor's proposal to use Medicaid expansion funds to provide health insurance to people who are currently not covered by Medicaid and who do not earn enough to qualify for subsidies.
The report offered the following conclusions and recommendations:
There is a lot of uncertainty related to the Healthy Utah plan. Usually the presence of uncertainty argues for exercising caution. Shouldn’t the state exercise caution in moving forward on bold, new plans?
Yes. But caution does not mean inaction. The costs to inaction in this case are millions of dollars in foregone benefits to state residents with each passing week. Those losses are certain, and they are not coming back.
The ACA is drastically re‐shaping American health care. Most Utahns, according to opinion polls, believe these changes are not for the better. But the state has no power to undo the ACA or to ignore its requirements or the taxes associated with it.
What the state does have the power to do is reclaim part of the funds that state residents are already contributing to fund the ACA. The Healthy Utah plan may or may not be the ideal option to make that happen, but it clearly brings hundreds of millions of dollars into the state to help low‐income residents who have no other means of obtaining health insurance. It does so at minimal risk to state budgets and at considerable gain to the state economy.
The economic case for moving forward with Healthy Utah at this time is compelling. Policymakers can move forward with confidence—even with the uncertainty that faces us.
Download the complete report here:
The Economics of the Healthy Utah Plan: A Preliminary Analysis
A Two-Generation Strategy: Right from the Start
Download and print the issue brief here:
A Two Generation Strategy: Right from the Start
This is the second in a series of issue briefs focused on two-generation strategies to reduce poverty supported by Ascend: the Aspen Institute.
The first issue brief in this series is available here:
A Two-Generation Approach to Ending Poverty in Utah
Full Text
A two-generation, multi-intervention strategy for single, first-time pregnant women in poverty is being developed by Salt Lake County. The three proposed interventions are:
• Nurse Family Partnership
• Education and training for the mother, and
• Two years of high quality preschool for the child beginning at 3 years of age
This combination of interventions is intended to improve the health of the mother and baby, reduce toxic stress, improve child welfare, economic self-sufficiency and the long term life prospects of the child.
COLLABORATION AND INNOVATION
Salt Lake County, the largest in Utah with a population of 1,032,2261, is planning to expand access to the Nurse Family Partnership (NFP). According to the County, approximately 1,100-1,500 women meet the eligibility requirements for NFP. However, only 100 women are currently being served.
Nurse Family Partnership is an evidenced-based community health program that provides ongoing home visits from pregnancy through age 2 of the child by a registered nurse to low-income, first time mothers to provide the care and support that they need to have a healthy pregnancy, be a responsible and caring parent, and to become more economically self-sufficient. Outcomes associated with NFP include long-term family improvements in health, child welfare, education and self-sufficiency.
More than 35 years of evidence from randomized, controlled trials prove this maternal health program’s effectiveness guiding low-income, first-time moms and their children to successful futures. By developing strong family foundations, the Nurse Family Partnership establishes better, safer, and stronger communities for generations to come.
NFP assists clients in returning to their local high school, alternative high school (which usually offers childcare services), or obtaining a GED. They help them with their college applications and suggest ways to finance schooling either through scholarships or PELL grants. NFP also works with the Utah Department of Workforce Services (DWS) Education and Training programs. The nurses encourage their clients to utilize programs which assist financially with completion of a high school diploma, GED, or ESL. NFP encourages participants to use DWS career planning services, take advantage of DWS financial incentives for setting and achieving educational goals, as well as assistance with childcare while
completing their education.
To supplement the education and training referrals performed by NFP, Salt Lake County plans to collaborate with the public libraries to offer Career Online High School to NFP participants in order to promote higher educational attainment and economic self-sufficiency. Career Online High School offers students the opportunity to earn an accredited high school diploma while learning real-world career skills. An accredited, private online school district, Career Online High School is specifically designed to re-engage adults into the education system and prepare them for entry into post-secondary education or the workforce. It is committed to preparing students for careers and post-secondary career education by delivering high-quality, supportive, and career-based online education. Career Online High School gives students the opportunity to earn an accredited high school diploma and credentialed career certificate. Students graduate with the tools to take the next step in their careers or career-education.
COLLABORATION BETWEEN SALT LAKE COUNTY AND THE DEPARTMENT OF WORKFORCE SERVICES
Salt Lake County and DWS will partner to expand access to Nurse Family Partnership, as well as education, training and employment opportunities for the participants. Through the intergenerational poverty focus of DWS, eligible women in Salt Lake County and those classified as living in “intergenerational poverty” will be the target population for the expansion. Additionally, DWS is interested in using Temporary Assistance for Needy Families (TANF) funds to increase access to NFP for this population.
FINANCING STRATEGY
Currently, funding for NFP in Salt Lake County is provided by County funds, Title V-Maternal and the Child Health Block Grant, a grant from the Department of Child and Family Services through the Community-Based Child Abuse Prevention (CBCAP) federal funding, and the Maternal, Infant and Early Childhood Home Visiting (MIECHV) Program created by the Patient Protection and Affordable Care Act of 2010.
To fund the expansion of NFP, Salt Lake County is exploring a blended funding strategy utilizing County funds, federal TANF funds through the collaboration with DWS, and investor funds through an innovative strategy called “Pay-for-Success” or social impact financing.
Under a “Pay-for-Success” financing model, there is an arrangement between one or more government agencies and an external organization where the government specifies the outcomes and promises to pay the external organization a pre-agreed amount if it is able to achieve the outcomes.3 Private commercial and philanthropic investors provide the upfront capital through the external organization to expand services for proven interventions with effective track records that either achieve desired outcomes and/or reduce the cost of later services to government. Outcome measures, such as reduction in preterm births and the spacing of second births, as well as reductions in other areas such as child maltreatment and criminal justice, in the case of NFP, are established and agreed upon by the parties. If the performance measures are achieved, the County would pay back the investors with interest. However, if the outcomes are not achieved, the investors may lose all or some of their investment. Several states, including North Carolina and New York State, and local jurisdictions, such as San Francisco, are exploring the expansion of NFP through social impact financing.
Salt Lake County participated in a proof of concept Results-Based Financing contract (a local term for Pay for Success) for high quality preschool in Utah for the 2013-2014 school year. Six hundred children who were identified as economically disadvantaged were funded through a Pay-for-Success contract. Goldman Sachs Bank and J.B. Pritzker provided the upfront investment. The United Way of Salt Lake and Salt Lake County provided the funds to repay the investors based on the performance metric of reducing the number of children funded through the contract who will need special education services in k-6. The project was announced during the Clinton Global Initiative Conference in June 2013. It is the first social impact loan in the U.S. to finance preschool.
THE PAY FOR PERFORMANCE ACT
On July 30, 2014, U.S. Senator Orrin Hatch (R-Utah), Ranking Member of the Senate Finance Committee and Senator Michael Bennet (D-Colorado), member of the Senate Finance Committee, introduced the Pay-For-Performance Act. The legislation is a companion bill to the Young-Delaney Social Impact Bond Act in the House of Representatives. The Pay-for-Performance Act directs resources to states and local communities to support innovative public-private partnerships to tackle social and public health challenges, while ensuring a smarter, more efficient use of tax dollars.
“The Pay-for-Performance Act gives policymakers a critical, evidence-based strategy for dealing with major societal challenges. By connecting the tools of impact investing to a ‘what works’ approach, this bill takes us one step closer to a smarter, leaner, results focused government. Senators Bennet and Hatch should be commended for providing a bi-partisan, national blueprint for cross sector investments in the outcomes our communities and country need.” Melody C. Barnes, former Director, White House Domestic Policy Council.
CONCLUSION
Although every birth is a major event and every child warrants special attention, home visiting for first time, low-income expectant mothers and their infants is especially beneficial because it provides information and support early in family formation and improves a woman’s ability to effectively parent. Combining home visitation with additional educational and improved employment opportunities leverages positive outcomes for both the mother and the child.
Additionally, implementing or expanding home visiting programs may reduce costs and increase the efficiency of care delivery for managed care organizations (MCO’s) and other health insurance providers. Evidence based home visiting programs have been shown to reduce health care costs by preventing complications in pregnancy, reducing injuries and maltreatment, enhancing maternal and child health through prevention and early detection and promoting efficient use of the health care system.
Two-generation approaches such as Nurse Family Partnership that include providing education and training for mothers are examples of strategies to meet the needs of vulnerable children and their parents.
Voices for Utah Children is proud to be a part of the Aspen Institute Ascend Network. The goal of the
Aspen Institute Ascend Network is to mobilize empowered two-generation organizations and leaders
to influence policy and practice changes that increase economic security, educational success, social
capital, and health and well-being for children, parents, and their families.
Learn more at http://ascend.aspeninstitute.org/network
Utah Kids Count Data Book
Current Utah KIDS COUNT Data Book
Measures of Child Well-Being, 2015
Previous Utah KIDS COUNT Data Books
KIDS COUNT Policy Reports
Creating Opportunity for Families: A Two-Generation Approach, 2014
Early Reading Proficiency in the United States, 2014
The First Eight Years: Giving Kids a Foundation for Lifetime Success, 2013
Utah Data Briefs
& Other Utah Data Products
A Two-Generation Strategy: Healthy Parents and Healthy Kids, 2014
Attendance and the Early Grades: A Two-Generation Issue, 2014
A Two-Generation Strategy: Right from the Start, 2014
A Two-Generation Approach to Ending Poverty in Utah, 2014
Kids Count in Utah Poster, 2013
Utah's Poverty Data at a Glance, 2009
Risk Factors Among Children in Utah, 2009
Teen Pregnancy Issue Brief, 2008
Basic Family Budgets: How Much Does It Take To Get By, 2007
Then and Now: Ten Years of Child Well-Being in Utah, 2005