Newsroom
State Policy
The Utah Intergenerational Poverty Work and Self-sufficiency Tax Credit
Planned pregnancies are healthier pregnancies.
New factsheets by the University of Utah School of Medicine describe two policy solutions that would help Utah families obtain healthcare they need to plan and space their pregnancies in order to better achieve the best health outcomes for the mother and child. In addition to promoting health, these solutions are cost-effective.
A Medicaid State Plan Amendment (SPA) allows family planning coverage for individuals that do not qualify for full Medicaid benefits. Expanding family planning coverage would maximize the the federal match and support the health of Utah families. There are 28 states that take advantage of the option to offer family planning coverage for individuals that do not qualify for full Medicaid benefits. These existing programs have proven to be budget neutral or cost-saving.
Long-acting reversible contraceptives (LARC) are highly effective contraception devices with minimal side effects that can be safely inserted immediately following delivery or during the mother's hospital stay. However, current Medicaid reimbursement procedures create a disincentive to offering LARC in this context. Unbundling LARC insertions from the global fee could improve access to this effective option.
For more information, see the complete fact sheets:
![]() Expanding Family Planning Coverage with Medicaid
Expanding Family Planning Coverage with Medicaid
![]() Expanding Options for Postpartum Contraception
Expanding Options for Postpartum Contraception
For 30 years now, Voices for Utah Children has called on our state, federal and local leaders to put children’s needs first. But the work is not done. The children of 30 years ago now have children of their own. Too many of these children are growing up in poverty, without access to healthcare or quality educational opportunities.
How can you be involved?
Make a tax-deductible donation to Voices for Utah Children—or join our Network with a monthly donation of $20 or more. Network membership includes complimentary admission to Network events with food, socializing, and opportunity to meet child advocacy experts. And don't forget to join our listserv to stay informed!
We look forward to the future of Voices for Utah Children and we hope you will be a part of our next 30 years.
Special thanks to American Express, our "Making a Difference All Year Long" sponsor. 
In Support of Medicaid Standards for Children
Why We Care About Medicaid “EPSDT” Benefits
and So Should You
While threats to the Affordable Care Act (ACA) may seem the most imminent in our current political landscape, Medicaid is also under attack. Congress and the new administration are discussing deep cuts and changes to the Medicaid program, through Medicaid block grants or per capita program caps. The new administration recently said they will be proposing block grants.
Medicaid block grants result in funding cuts and fewer people receiving coverage. Utah has long been recognized as a leader in health care innovation, but our ability to innovate will be severely impaired if we experience cuts to our foundational health care safety-net system through block grants. Medicaid is the cornerstone to children’s health coverage in Utah.
In a recent letter to Congress on January 13th, the Governor and state officials weighed in on a number of health reform proposals, including Medicaid. We saw many areas for concern in our state leaders’ letter; one brief recommendation in particular jumped out at us, because it would have significant and long-lasting consequences for children and families:
“Reevaluate the EPDST (Early Period Screening, Diagnosis and Treatment) benefit for children. EPDST requires states to provide comprehensive and preventative health services for Medicaid beneficiaries under the age of 21 with few limitations.
Consider limiting benefits to what is available in the private market. Currently, children on Medicaid have more access to services and benefits than children who are covered under good commercial plans.”
So, what is EPSDT?
Early, Periodic Screenings, Diagnosis & Treatment
 The EPSDT benefit, known in Utah as “CHEC” or Children’s Health Evaluation and Care, is one of the hallmarks of the Medicaid program. The Medicaid Act currently requires states to provide children with a comprehensive scope of services. For decades, EPSDT has allowed providers to catch potential health problems early, when they are easiest to treat and children stand the best chance of developing to their fullest potential. Covered EPSDT services include basic preventative care, such as dental and vision services, plus services needed to address acute, long-term, and disabling conditions, such as physical, speech and behavioral health therapies and in-home nursing. The EPSDT benefit is considered the gold standard for children’s pediatric benefits. It helps doctors determine the best level of care for their patient.
The EPSDT benefit, known in Utah as “CHEC” or Children’s Health Evaluation and Care, is one of the hallmarks of the Medicaid program. The Medicaid Act currently requires states to provide children with a comprehensive scope of services. For decades, EPSDT has allowed providers to catch potential health problems early, when they are easiest to treat and children stand the best chance of developing to their fullest potential. Covered EPSDT services include basic preventative care, such as dental and vision services, plus services needed to address acute, long-term, and disabling conditions, such as physical, speech and behavioral health therapies and in-home nursing. The EPSDT benefit is considered the gold standard for children’s pediatric benefits. It helps doctors determine the best level of care for their patient.
EPSDT has helped millions of children, especially children with special health care needs, receive the level of the care they need. In fact, many families in the private insurance market will turn to Medicaid coverage for their children with special health care needs-- because they cannot afford such comprehensive benefits in their “good” commercial plan.
We Need to Protect EPSDT
Medicaid is the cornerstone for children’s health coverage in our state, and serves over 20% of our most vulnerable families. If we roll-back the EPSDT benefit, we will see a surge of parents no longer able to afford care, particularly for children with special health care needs.
EPSDT protects families; it assures families that they can receive a minimum level of coverage and have access to services that meet prevailing standards of care. For many higher-income families, Medicaid may seem unconnected to their day-to-day lives. But one of the core tenets of our health care safety-net is that it is there for families when they need it.
There are many improvements needed to our Medicaid program. But the EPSDT benefit package is not one of them. So why fix what isn’t broken? Instead, for example, Medicaid mental and behavioral health services should be better integrated and aligned with physical health benefits.
Instead of trying to raise health care standards for all kids, our state and federal leaders are instead looking to dilute standards. It is perverse logic to limit progress and roll-back gains, in order to achieve equality. Instead we should advance the progress made so all children can achieve affordable, comprehensive coverage.
We urge our state and federal leaders:
Do not limit benefits for children and weaken our existing standards.
Build on the progress we have made.
Strengthen coverage and care for all Utah children.
For 30 years now, Voices for Utah Children has called on our state, federal and local leaders to put children’s needs first. But the work is not done. The children of 30 years ago now have children of their own. Too many of these children are growing up in poverty, without access to healthcare or quality educational opportunities.
How can you be involved?
Make a tax-deductible donation to Voices for Utah Children—or join our Network with a monthly donation of $20 or more. Network membership includes complimentary admission to Network events with food, socializing, and opportunity to meet child advocacy experts. And don't forget to join our listserv to stay informed!
We look forward to the future of Voices for Utah Children and we hope you will be a part of our next 30 years.
Special thanks to American Express, our "Making a Difference All Year Long" sponsor. 
Healthy Teeth = Healthy Kids!
Oral Health Care for Children and Families
 Tooth decay is the top preventable disease for kids. When kids experience poor oral health, their school attendance and grades are likely to suffer. Kids experiencing dental pain cannot concentrate in school and fully participate in activities. What’s more, oral health decay can lead to other serious medical problems. An estimated 65% of Utah children have experienced a dental cavity by the time they are 9-years-old.
Tooth decay is the top preventable disease for kids. When kids experience poor oral health, their school attendance and grades are likely to suffer. Kids experiencing dental pain cannot concentrate in school and fully participate in activities. What’s more, oral health decay can lead to other serious medical problems. An estimated 65% of Utah children have experienced a dental cavity by the time they are 9-years-old.
The best way to treat cavities is through prevention: we can prevent oral health problems before they occur. But many families have trouble accessing affordable dental care for their kids. Working parents may not be able to get the time off for a routine visit. Low-income children, children of color and children in rural areas have an even harder time accessing a dentist in their communities. According to a recent Department of Health report, Hispanic children were five times more likely to report having unmet dental health needs compared to White children.
School-based prevention or sealant programs are one of the best ways to ensure all kids can receive affordable, preventative oral health care.
We need to help more children access school-based sealant programs and affordable care. Voices for Utah Children supports policies that expand dental care access for all children including:
- Changes to the Utah Medicaid dental program to better meet the needs of low-income families and expand school-based care, including reimbursing for patient assessment in a public health settings (Medicaid code D0191).
- Expanding Medicaid and CHIP oral health quality performance measures, monitoring and evaluation to improve kids’ utilization of preventive care visits.
- Expanding dental health benefits for children in the marketplace, including a more robust pediatric dental benefit package and embedding children’s dental health benefits into all plans.
- A comprehensive state plan to address oral health access disparities experienced by low-income children, children of color, and children in rural areas across the state.
Our children should not be falling behind due to cavities or oral health pain. Together we can strengthen our pediatric oral health system so all kids can succeed.
Image Credit: © Oksun70 | Dreamstime.com - Kid Girl Brushing Teeth In Bathroom Photo
Image Credit: American Dental Association
For 30 years now, Voices for Utah Children has called on our state, federal and local leaders to put children’s needs first. But the work is not done. The children of 30 years ago now have children of their own. Too many of these children are growing up in poverty, without access to healthcare or quality educational opportunities.
How can you be involved?
Make a tax-deductible donation to Voices for Utah Children—or join our Network with a monthly donation of $20 or more. Network membership includes complimentary admission to Network events with food, socializing, and opportunity to meet child advocacy experts. And don't forget to join our listserv to stay informed!
We look forward to the future of Voices for Utah Children and we hope you will be a part of our next 30 years.
Special thanks to American Express, our "Making a Difference All Year Long" sponsor. 
Preserve and Protect Health Coverage for Utah Children and Families
Medicaid, CHIP (the Children’s Health Insurance Program) and the Affordable Care Act (ACA) form the foundation of children’s health coverage. These programs are deeply connected to one another and our overall state safety net system. Federal and state lawmakers are proposing and enacting proposals that undermine ACA, CHIP and Medicaid. A repeal, cut or restructure of one program affects the others, and puts the care of Utah children and families at risk.
Thanks to the ACA, Medicaid and CHIP, we have seen the rate of uninsured Utah children drop from 11% in 2011 to a historic low of 6% in 2016. We cannot afford to let child health coverage, adequacy, and affordability move backwards. We must ensure that we sustain and build on our unprecedented success in covering children.
Medicaid is the cornerstone for children’s health coverage. Our state leaders must support the continued stability and affordability of the Medicaid program. Medicaid is the safety net health care program for low-income children. Over 200,000 Utah children rely on Medicaid insurance coverage, and its pediatric benefits are considered the gold standard for child health, particularly for children and youth with special health care needs. Changes to Medicaid’s financing structure through a block grant or per capita cap would undermine the program’s integrity by creating gaps in state funding. They would likely lead to limits placed on the programs, such as a reduction in benefits or fewer kids covered. Proposals to promote state innovation need to strengthen our safety net for kids and families, not weaken it.
Block grants or per capita caps would undermine Medicaid program integrity. Changes to Medicaid’s financing structure through a block grant or per capita cap would create large shortfalls in state funding. Learn more about h ow block grants would harm Utah's budget.
ow block grants would harm Utah's budget.
Extend funding for CHIP for at least five years. A robust, long-term extension of CHIP funding for at least five years would help stabilize coverage for the 8.9 million U.S. children who rely on CHIP and provide certainty to Utah amid potentially significant changes to the broader coverage landscape. Learn more about CHIP.
Children must not lose any ground. Unraveling the ACA without a replacement plan attached threatens the health of children and families. There are 38,000 Utah children enrolled in ACA, or marketplace, coverage. At least 87% of Utahns enrolled in the exchange are receiving subsidies. The ACA provides protections for children and families, increases affordability and establishes evidence-based essential health benefits.
Extend Medicaid Coverage for Parents. Medicaid coverage for parents benefits the whole family. Yet thousands of Utah families are unable to receive Medicaid coverage, falling into the Medicaid ‘coverage gap.’ As a result, the family is at increased financial risk. Moreover, children are more likely to be uninsured. It is time to close the coverage for all parents and individuals. Learn more about citizen initiatives to close the coverage gap.
Working families depend on these vital health care programs. What is at stake if the ACA is repealed without a replacement, or changes are made to CHIP and Medicaid?
- The number of uninsured Utah children would more than double. By 2019, at least 141,000 children would be uninsured.
- The number of uninsured Utah parents would jump from 82,000 to 171,000. Research shows that children are better off when their parents have health insurance coverage.
- Families and individuals would lose protection from exclusions and discrimination. Approximately 1.2 million Utahns – including 411,000 children- no longer experience lifetime limits on coverage now that the ACA is in effect.
We are putting our children’s future at risk by failing to guarantee Utah children and families have stable health insurance coverage. All children and families need consistent, comprehensive and affordable care.
Medicaid Helps Utah Children Get the Health Care They Need to Succeed from Georgetown CCF on Vimeo.
Printer-friendly Version:
![]() Preserve and Protect Health Coverage for Utah Children and Families
Preserve and Protect Health Coverage for Utah Children and Families
Additional Materials
Utah Children and the Terrible, Horrible, No Good, Very Bad Healthcare Repeal Bill
In Support of Medicaid Standards for Children
Block grants or per capita caps would undermine the Medicaid program.
Number of Uninsured Utah Kids and Parents Would More than Double if ACA Repealed
The ACA Gave a Needed Boost to Utah’s Latino Child Health Insurance Rate
Tell Senator Hatch Not to Repeal the ACA without Replacing It
Defending Health Care in 2017: What Is at Stake for Utah
273,000 Utah Residents Would Lose Coverage in 2019 Under ACA Repeal2019 Under ACA Repeal
What Would Block Grants or Limits on Per Capita Spending Mean for Medicaid?
Fact Sheet: Per Capita Caps vs. Block Grants in Medicaid
For 30 years now, Voices for Utah Children has called on our state, federal and local leaders to put children’s needs first. But the work is not done. The children of 30 years ago now have children of their own. Too many of these children are growing up in poverty, without access to healthcare or quality educational opportunities.
How can you be involved?
Make a tax-deductible donation to Voices for Utah Children—or join our Network with a monthly donation of $20 or more. Network membership includes complimentary admission to Network events with food, socializing, and opportunity to meet child advocacy experts. And don't forget to join our listserv to stay informed!
We look forward to the future of Voices for Utah Children and we hope you will be a part of our next 30 years.
Special thanks to American Express, our "Making a Difference All Year Long" sponsor. 
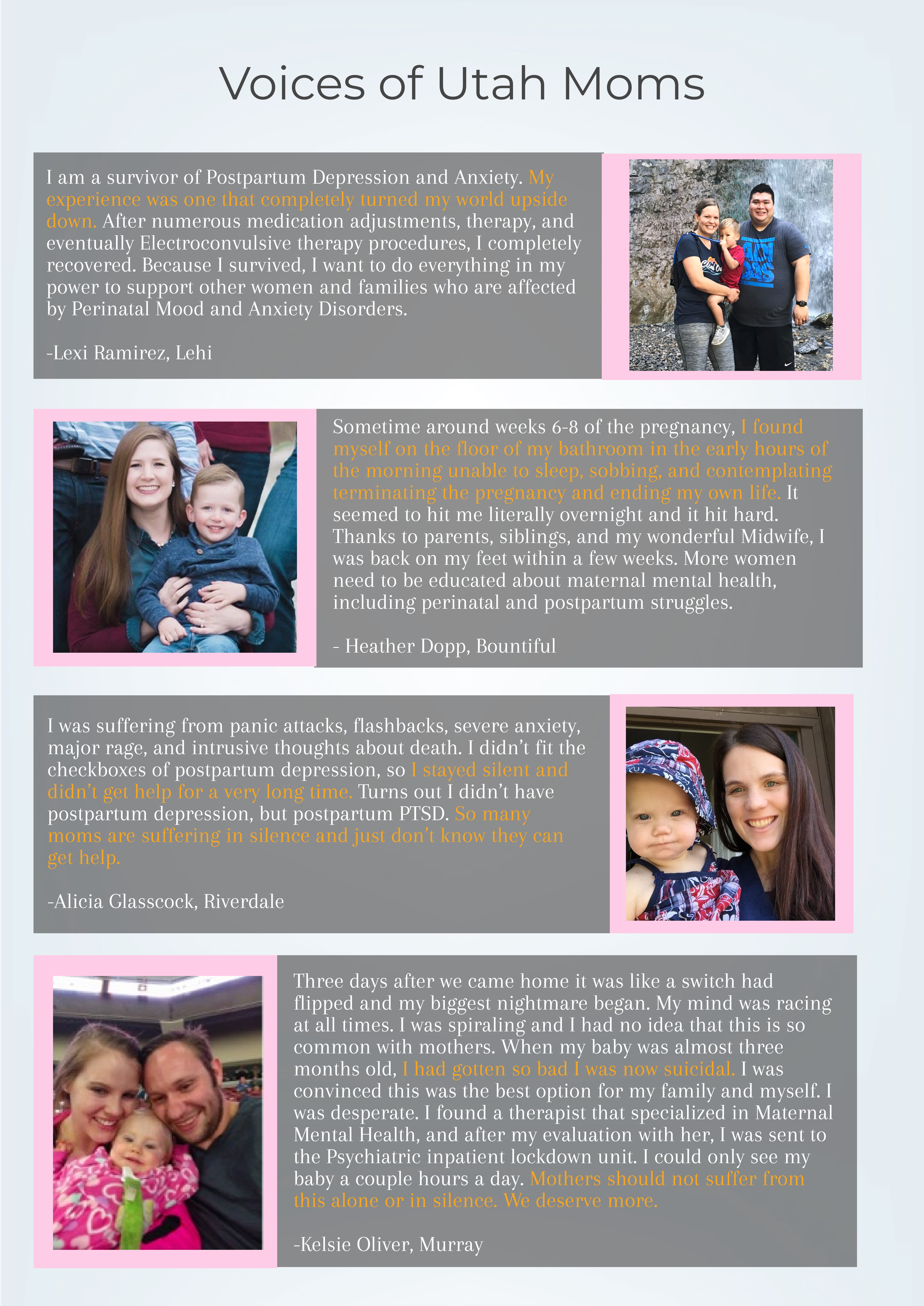
Healthy Moms = Healthy Kids
For Printable Version ![]() Maternal Mental Health Support Flyer
Maternal Mental Health Support Flyer
For 30 years now, Voices for Utah Children has called on our state, federal and local leaders to put children’s needs first. But the work is not done. The children of 30 years ago now have children of their own. Too many of these children are growing up in poverty, without access to healthcare or quality educational opportunities.
How can you be involved?
Make a tax-deductible donation to Voices for Utah Children—or join our Network with a monthly donation of $20 or more. Network membership includes complimentary admission to Network events with food, socializing, and opportunity to meet child advocacy experts. And don't forget to join our listserv to stay informed!
We look forward to the future of Voices for Utah Children and we hope you will be a part of our next 30 years.
Special thanks to American Express, our "Making a Difference All Year Long" sponsor.